Why blunt?
1. Reduced risk of intraneural or worse intrafascicular injection. Likely the primary cause of serious nerve injury from peripheral nerve blocks.
2. Reduced risk of intravascular injection and resulting systemic local anesthetic toxicity
3. Reduced risk of inadvertent subarachnoid needle placement when performing proximal blocks such as the interscalene brachial plexus block. Total spinal anesthesia and devastating spinal cord syrinx formation has been reported.
Our block needle lineup
Our new blunt tip block needles! Ease of use, safe and allows for easy hydrodissection with NS
"Blunt tip" 22G block needle for brachial plexus blocks in the neck and all purpose shallow target blocking.
Quincke tip spinal (20-22G) is a back up if a block needle is unavailable. Notice bevel is very similar to "blunt tip" block needles. We use both the standard length and the shorter 1.5inch length depending on target nerve depth.
*Never use a long needle if there is a high-risk deep structure, for example interscalene blocks should be performed with short needles only.Touhy epidural needle for deeper blocks--infraclavicular brachial plexus, femoral, popliteal sciatic etc...
Terrifying central cord syrinx reported after an interscalene block with a too deep (subarachnoid) injection
When does needle choice really matter?
Brachial plexus blocks! Large monofasicular nerves are clearly at greater risk for intraneural needle tip placement. A blunt tip block needle that is short (1-2 inches) should be used whenever possible. There is no definitive data to guide us here, but expert opinion is clear, proximal blocks such as the interscalene brachial plexus block are relatively higher risk for needle to nerve injury and a larger bore, blunt tip needle likely improves safety. .
We use a 22G blunt tip block needle with a small stopper to prevent deep injection (subarachnoid placement )
Popliteal Sciatic blocks. Here the imaging can be tricky and close needle to nerve placement often necessary for a successful block. Having a blunt needle tip helps reduce risk of harm when needling very close to the nerve. In addition, there are large vessels, easily compressed and missed while scanning, increasing the risk for intravascular injection.
We use a 20G Touhy needle with blunt tip to reduce risk of needle-to-nerve injury, inadvertent intrafasicular placement, and inadvertent intravascular injection.
What about femoral blocks? There is no reason to be anywhere near to the femoral nerve for this block. Needling close to the nerve itself, versus in the sub-fascia iliaca plane adds risk without benefit. Thus, improving block safety should be accomplished primarily by needle placement being at least 1-2cm lateral to the femoral nerve.
We use a 20G Touhy needle with blunt tip to reduce risk of needle-to-nerve injury, inadvertent intrafasicular placement, and inadvertent intravascular injection.
Can I ever use a "sharp" needle for blocks?
The most conservative answer is "No." However, the realistic risk of intra-fasicular injection and nerve injury with radian, ulnar, and median blocks at the forearm and posterior tibial / other ankle blocks is likely very very low.
If I don't have a block needle, should I not perform blocks?
Yes with great caution. We are emergency providers, if we have to intubate with a tongue depressor to save a life, that is what we will do. Dealing with a less than ideal set up is what we are trained to manage.
BUT ....
When available, don't over think this issue--use a blunt tip needle. When a block needle is unavailable, here are some things that can be done to reduce risk of nerve injury.
You should always have a Quincke spinal needle to use. Avoid standard hypodermic needles.
From the image above, you can see the difference in bevel angle of a commonly available Quincke tip spinal needle and a "block needle" is very small. For that reason, we believe it is defensible to use a Quincke tip spinal needle of appropriate length--i.e. no long needles in the neck EVER--with a meticulous, "stay-away" technique where any needle to nerve contact is conscientiously avoided with real-time ultrasound-guidance.
Other Tips for Reducing risk of needle-to-nerve injury
Only block an awake and calm patient: Any parasthesias or pain with needling while using a non-block needle should be be considered high risk events prompting movement away from any nerve, ceasing any injection, and potentially aborting the procedure all together. Intoxicated patients make unpredictable moves that are risky; patient should be awake and calm.
Use In-plane US visualization of the entire needle shaft
Avoid high risk blocks--interscalene brachial plexus in particular--unless you have 100% confidence in your needle visualization and anatomy. No fishing around in a large neck with sketchy imaging.
Use a Stay-away technique maximizing the distance from needle to nerve.
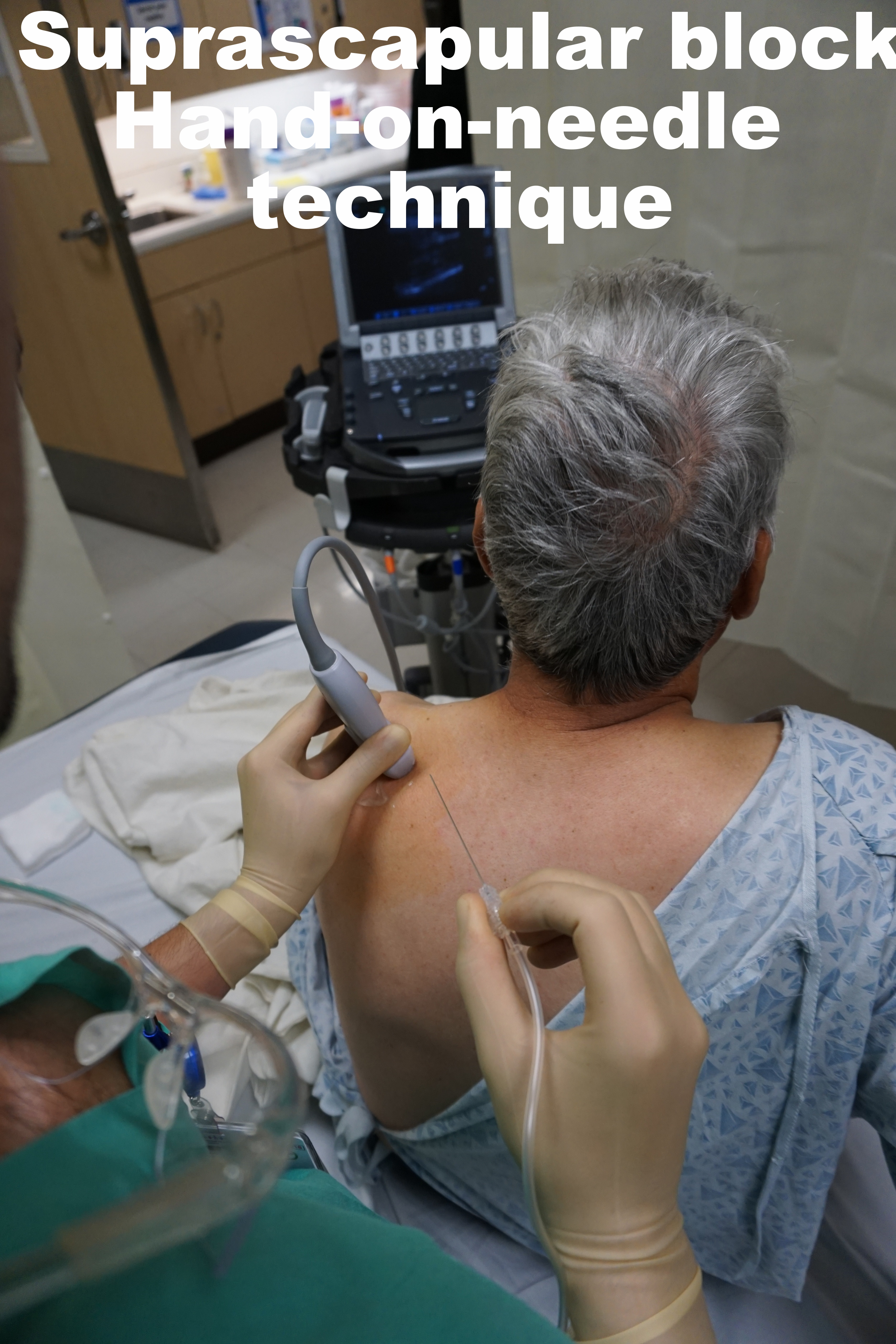
Use hand-on-needle, two-person technique. More control, better ergonomics likely translate into a safer block.
Use Pressure monitoring
One problem with blunts
Further Reading
Neal, Joseph M., et al. "ASRA practice advisory on neurologic complications in regional anesthesia and pain medicine." Regional anesthesia and pain medicine 33.5 (2008): 404-415.
Benumof JL. Permanent loss of cervical spinal cord function associated with interscalene block performed under general anesthesia.Anesthesiology. 2000;93:1541-4.
Cohen JM, Gray AT. Functional deficits after intraneural injection during interscalene block. Reg Anesth Pain Med. 2010;35:397-9.
Hadzic A, Dilberovic F, Shah S, et al. Combination of intraneural injection and high injection pressure leads to fascicular injury and neurologic deficits in dogs. Reg Anesth Pain Med. 2004;29:417-23.
Liu SS, Yadeau JT, Shaw PM, Wilfred S, Shetty T, Gordon M. Incidence of unintentional intraneural injection and postoperative neurological complications with ultrasound-guided interscalene and supraclavicular nerve blocks. Anaesthesia. 2011;66:168-746.
Rice AS, Mcmahon SB. Peripheral nerve injury caused by injection needles used in regional anaesthesia: influence of bevel configuration, studied in a rat model. Br J Anaesth. 1992;69:433-8.
Selander, Dag, Karl‐Gustav Dhunér, and Göran Lundborg. "Peripheral nerve injury due to injection needles used for regional anesthesia." Acta Anaesthesiologica Scandinavica 21.3 (1977): 182-188.
Steinfeldt T, Poeschl S, Nimphius W, et al. Forced needle advancement during needle-nerve contact in a porcine model: histological outcome. Anesth Analg. 2011;113:417-20.
Tsui, Ban CH, Mark P. Knezevich, and Jennifer J. Pillay. "Reduced injection pressures using a compressed air injection technique (CAIT): an in vitro study."Regional anesthesia and pain medicine 33.2 (2008): 168-173.